Sohar Health
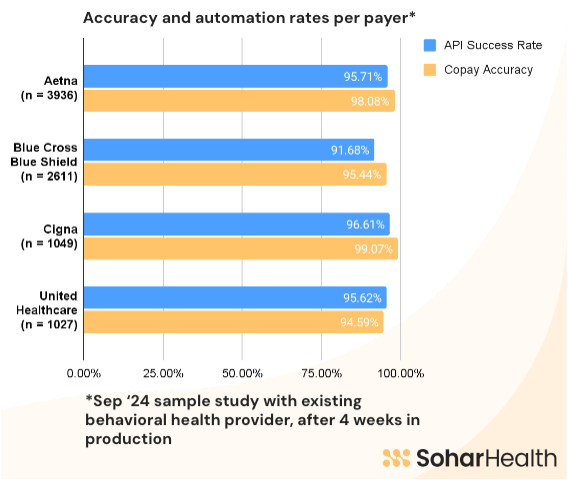
Sohar Health delivers the industry-leading front end RCM automation solution with unmatched accuracy and efficiency. We excel in reducing claims denials, maximizing revenue, and cutting costs through automated eligibility and Verification of Benefits. Our market-leading outcomes include the highest payer accuracy for benefits data (>95% across copay and coinsurance), rapid checks (>90% return of checks < 30 seconds), and seamless API integration, all with unparalleled reliability.
About
Sohar Health offers a comprehensive suite of front end RCM solutions designed to optimize patient intake, revenue cycle management while reducing operational inefficiencies, and insurance claims denials.
Our platform is built to deliver the strongest outcomes in the market, helping healthcare organizations minimize claims denials, maximize revenue, and streamline manual workflows for significant cost savings. We provide a high level of accuracy across payers (>95% across copays and coinsurances) and automation (>90% of checks returned in under 30 seconds), ensuring that your patients will receive reliable cost estimations faster during their onboarding experience.
API Solutions:
1. Eligibility and Verification of Benefits: Instantly verify patient eligibility and confirm benefit details with high accuracy across various payers (>95% across copays and coinsurances). Our API ensures quick, reliable access to real-time information, reducing the risk of denials due to coverage issues.
2. Insurance Coverage Discovery: Our coverage discovery API identifies unknown or unreported insurance coverage (>60% discovery hit rate), increasing your chances of taking on a new patient and billing to their insurer, or finding the payer for a patient with lapsed coverage.
3. Network Status Determination: Easily determine whether your providers are in-network or out-of-network with our API.
4. Patient Responsibility Calculation: Accurately calculate patient responsibility using our advanced API, ensuring precise estimations of upfront costs, leading to better payment collections and improved pricing transparency for patients.
With seamless API integration, rapid check speeds, and a highly reliable platform, Sohar Health is your trusted partner for optimizing revenue cycle management and achieving better financial outcomes.
Our platform is built to deliver the strongest outcomes in the market, helping healthcare organizations minimize claims denials, maximize revenue, and streamline manual workflows for significant cost savings. We provide a high level of accuracy across payers (>95% across copays and coinsurances) and automation (>90% of checks returned in under 30 seconds), ensuring that your patients will receive reliable cost estimations faster during their onboarding experience.
API Solutions:
1. Eligibility and Verification of Benefits: Instantly verify patient eligibility and confirm benefit details with high accuracy across various payers (>95% across copays and coinsurances). Our API ensures quick, reliable access to real-time information, reducing the risk of denials due to coverage issues.
2. Insurance Coverage Discovery: Our coverage discovery API identifies unknown or unreported insurance coverage (>60% discovery hit rate), increasing your chances of taking on a new patient and billing to their insurer, or finding the payer for a patient with lapsed coverage.
3. Network Status Determination: Easily determine whether your providers are in-network or out-of-network with our API.
4. Patient Responsibility Calculation: Accurately calculate patient responsibility using our advanced API, ensuring precise estimations of upfront costs, leading to better payment collections and improved pricing transparency for patients.
With seamless API integration, rapid check speeds, and a highly reliable platform, Sohar Health is your trusted partner for optimizing revenue cycle management and achieving better financial outcomes.
Features
Specific service eligibility determination
Ensure that patients are eligible for care delivery within the onboarding / intake flow, or prior to an upcoming appointment by retrieving active coverage information and eligibility determination on a specific service basis
Medicare / Medicaid supported
Sohar supports all commercial payers, as well as, Medicare and Medicaid patients. If you wish to use Sohar on such patients, please reach out to the operations team at Sohar via email ([email protected])
Payer intelligence and member ID routing
Minimize backend billing errors by receiving up-to-date information about your patients' data on record with the payer, including name, DOB, and address. Even with incorrect member ID / payer combinations, Sohar is still able to route requests to the appropriate payer to pick out the relevant benefits data.
Payer carve outs / TPAs identification
Reduce the risk of claims denials associated with patients being out of network, and ensure accurate billing with carve out and TPA identification (>90% identification of Magellan Health and Carelon)
Media
Pricing
Eligibility checks start from $0.40 per eligibility check (volume discounts may apply). Please message the Sohar Health team for further details
Sohar Health eligibility and verification API
$0.40 per API call
Up to 25,000 verifications per year
* The pricing here is for display purposes only. You should contact the partner for the most up to date and correct pricing information. We do not take any responsibility for this pricing information, which is provided by our partners. Pricing last updated: 17 Jan, 2025 12:00AM
Next Steps
Fill Out the Activate a Partner Form
To let Sohar and Healthie know that you're ready to activate the integration, please fill out this form.
Partner with Sohar
Before turning on your integration with Sohar, you'll need to sign an agreement with them. Click Learn More About Sohar above to get in touch with their team.
Testimonials
Resources
FAQ
Out of the box, we can support around 1,000 payers, including the commercial payers, Medicare, and Medicaid payers. For an up-to-date list of the payers that we support, send us an email at [email protected]
The vast majority of our checks (> 90%) are returned within 30 seconds of request.
However, sometimes it is the case that a payer's data connection is not working and we have to retry until we are able to retrieve the benefits - we continue to retry up to 24 hours after the request has been made to maximize the chance that we retrieve the benefits data.
In some cases, a payer does not have an automated data connection directly or via a clearinghouse, in these instances, our manual operations team can go onto a portal or call the payer to retrieve the benefits information. We guarantee to return this information within one working day. Note: there is an additional fee for manual resolutions of checks
However, sometimes it is the case that a payer's data connection is not working and we have to retry until we are able to retrieve the benefits - we continue to retry up to 24 hours after the request has been made to maximize the chance that we retrieve the benefits data.
In some cases, a payer does not have an automated data connection directly or via a clearinghouse, in these instances, our manual operations team can go onto a portal or call the payer to retrieve the benefits information. We guarantee to return this information within one working day. Note: there is an additional fee for manual resolutions of checks
Yes, absolutely - it is one of the key reasons why our customers get so much value out of Sohar. We surface if there is a benefit related entity or additional payer on record for an individual patient, so that you always know where you should be submitting a claim
Our starting price per eligibility request is $0.40. The price can be discounted depending on the volume of checks you expect to run per annum. We provide you with an allocation of checks for the year and bill you for this amount quarterly.
If you exceed your annual allocation of checks, no worries - we will bill you at your next invoicing cycle for overages (these are charged at the same negotiated rate per check).
If you exceed your annual allocation of checks, no worries - we will bill you at your next invoicing cycle for overages (these are charged at the same negotiated rate per check).
Sohar is a machine learning solution that uses claims data to train its models to determine the most accurate benefits to surface for a specific service. As a result, we have confirmed accuracy rates of 95% on average across copays and coinsurances across payers, such as Aetna and UHC.
If you use a clearinghouse, such as Waystar, or an existing billing vendor, such as Candid Health, we can ingest your claims data, and generate personalized reports for your organization, with no engineering lift on your side.
If you use a clearinghouse, such as Waystar, or an existing billing vendor, such as Candid Health, we can ingest your claims data, and generate personalized reports for your organization, with no engineering lift on your side.
At Sohar Health, the security and protection of sensitive data, including Protected Health Information (PHI), is a top priority. We are SOC 2 Type II certified, which ensures that we meet the highest standards for data security, availability, confidentiality, and privacy.
We implement advanced encryption methods, both at rest and in transit, to protect all data. Our systems are regularly audited for vulnerabilities, and we employ continuous monitoring to detect and prevent any unauthorized access or breaches. We adhere to all HIPAA guidelines, ensuring that PHI is handled with the utmost care, with access restricted to only those authorized to manage the information.
By combining strong security protocols with industry-leading certifications, Sohar Health guarantees that your data remains safe, secure, and compliant at all times.
We implement advanced encryption methods, both at rest and in transit, to protect all data. Our systems are regularly audited for vulnerabilities, and we employ continuous monitoring to detect and prevent any unauthorized access or breaches. We adhere to all HIPAA guidelines, ensuring that PHI is handled with the utmost care, with access restricted to only those authorized to manage the information.
By combining strong security protocols with industry-leading certifications, Sohar Health guarantees that your data remains safe, secure, and compliant at all times.
Sohar Health leverages advanced machine learning to optimize the accuracy and reliability of the benefits data we provide. Our AI system is designed to predict and surface the most accurate benefits information from 271 responses, ensuring that you receive precise and actionable data.
For transparency and customer control, all claims data files that we ingest are securely stored in dedicated S3 subdirectories, designated to each specific customer. The key data points we extract from these files can be clearly outlined, so you always know exactly what information is being utilized.
Importantly, the only data points used in model training are those directly related to benefits, such as copay, coinsurance, and deductible. Our machine learning model is trained on this data to assign probabilities to the benefits returned by the payer in the 271 response, improving the accuracy of the data without compromising privacy or over-relying on unnecessary information.
Through this approach, Sohar Health ensures that AI enhances your ability to manage revenue cycles with precision and reduce claim denials, while keeping your data secure.
For transparency and customer control, all claims data files that we ingest are securely stored in dedicated S3 subdirectories, designated to each specific customer. The key data points we extract from these files can be clearly outlined, so you always know exactly what information is being utilized.
Importantly, the only data points used in model training are those directly related to benefits, such as copay, coinsurance, and deductible. Our machine learning model is trained on this data to assign probabilities to the benefits returned by the payer in the 271 response, improving the accuracy of the data without compromising privacy or over-relying on unnecessary information.
Through this approach, Sohar Health ensures that AI enhances your ability to manage revenue cycles with precision and reduce claim denials, while keeping your data secure.
Typical implementation time for integration of our API is up to 4 weeks. With the Healthie integration in place, this process can be completed within days.
However, we will still connect you with our Customer Success team to ensure that we have fully mapped your contracted payer list to Sohar's, that you receive the appropriate training on how best to parse through data to Sohar, and to set up your claims data ingestion (for reporting purposes).
Typically, we do biweekly CS touch bases for 3 months post-contract signing, and then we move to quarterly meetings.
However, we will still connect you with our Customer Success team to ensure that we have fully mapped your contracted payer list to Sohar's, that you receive the appropriate training on how best to parse through data to Sohar, and to set up your claims data ingestion (for reporting purposes).
Typically, we do biweekly CS touch bases for 3 months post-contract signing, and then we move to quarterly meetings.