Customized Solutions to Expediate Claim Approvals
Efficient, Personalized Claim Management for Faster Reimbursement
About
ClaimRev is Native Woman Owned medical claims clearinghouse. We empower your team with innovative solutions designed to increase third-party reimbursements, reduce claim denial rates, and ensure data ownership and security.
Sharp Claim Processing
Sharp Claim Processing
- Seamless Claim Submissions: Claims are rigorously scrubbed and efficiently sent to payers.
- Clear ERA Insights: Receive human-readable ERA reports to simplify understanding and streamline reconciliation.
- HIPAA Compliance: Fully compliant with all HIPAA standards to ensure data security and privacy.
- Custom Analytics & Reporting: Tailored dashboards and analytics to meet your unique reporting needs.
- API Access: Easily integrate with your existing systems using our robust API.
- Efficient Workflows: Organize claims into distinct workflows to simplify managing rejections and reduce bottlenecks.
- Rules Engine: Advanced, customizable claim edits to ensure claims are accurately paid the first time.
Sharp Revenue Tools
- Integrated Real-Time Eligibility: Check patient eligibility in real time, directly within Healthie appointments, with access to over 2,000 payers.
- Comprehensive Eligibility Checks: Perform both real-time and batch eligibility verifications with thousands of payers through our portal.
- Coverage Discovery: Identify previously unknown insurance coverage for self-pay patients to maximize reimbursements.
Features
Responsive Customer Service
Our customer service team is easy to reach—just a quick phone call or email, and your questions are answered swiftly, with any issues resolved promptly. We're always here to support you and ensure your claims process runs smoothly.
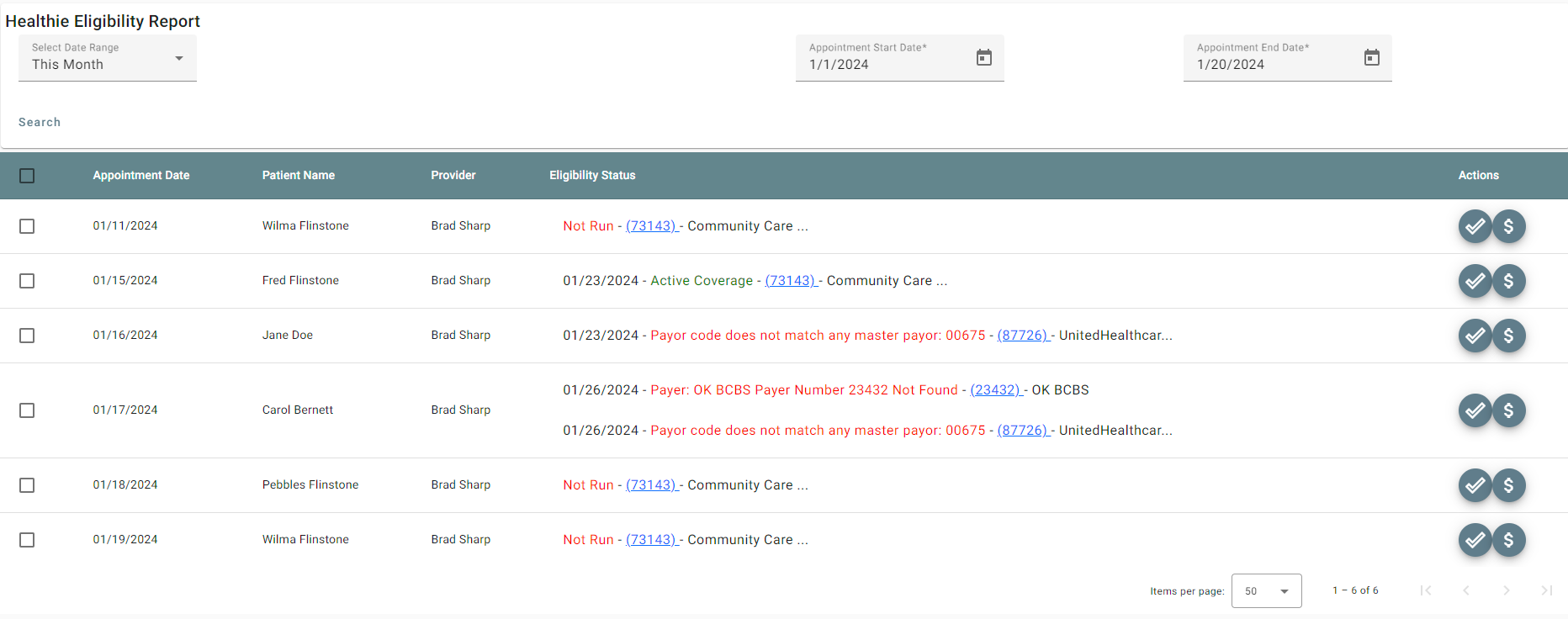
Pre-Appointment Coverage Verification with Integrated Eligibility Checks
Run reports for upcoming appointments to ensure patients have active coverage and the correct benefits, giving you confidence and clarity before they arrive.
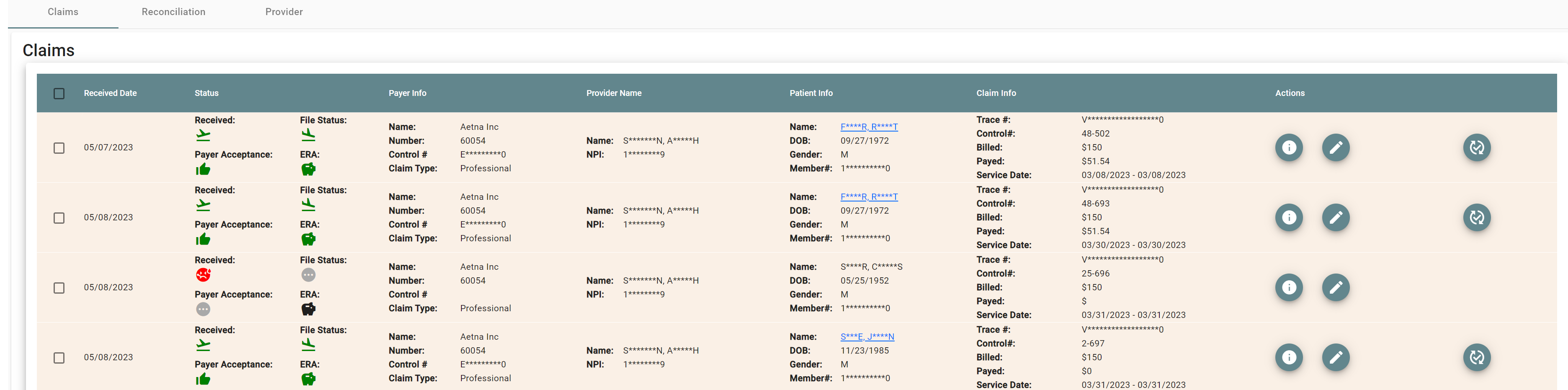
ERA Updates in Healthie
Once an ERA is returned, ClaimRev’s processing system updates your claim in Healthie with the payment details from the payer. The claim status is also refreshed, keeping you fully informed at every step of the reimbursement process.
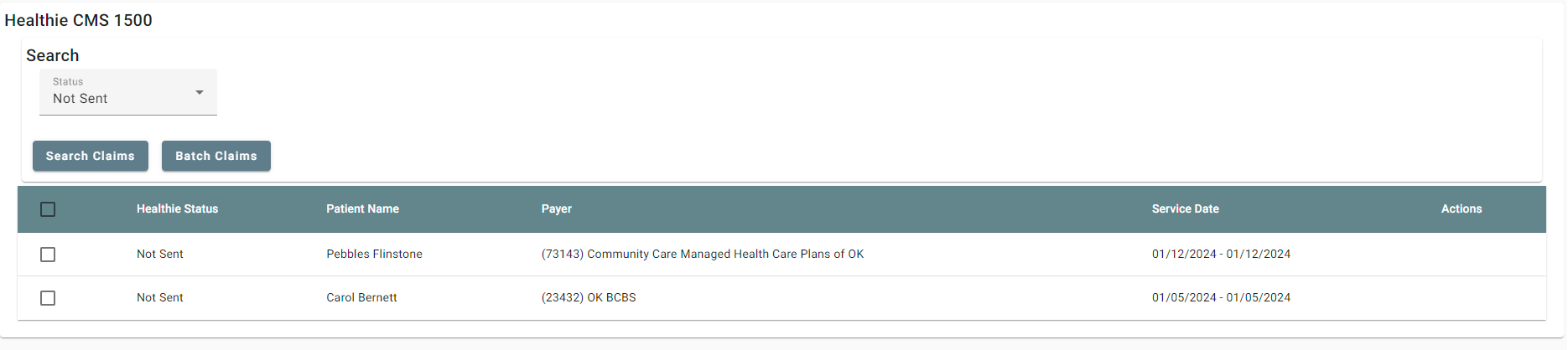
Effortless HCFA Claim Management
When HCFA claims are created in Healthie, our seamless integration allows them to be pulled into our processing system with a simple button push. Our advanced system then scrubs each claim for errors, ensuring only clean claims are sent to the payer. Throughout this process, we keep your Healthie account updated, so you’ll always know the status of your claims—from receipt to submission to the payer!
Media
Pricing
NEW Limited Time Tiered Provider Pricing!
$40
Pricing Tier for Rendering Providers
1 to 2 Providers: $50 per provider
3 to 10 Providers: $40 per provider
11+ Providers: $35 per provider
- If a practice has 9 providers, each provider would be priced at $40.
- This tiered structure offers discounts as the number of providers increases, making it more cost-effective for practices with higher provider counts.
Standard Pricing
50Per Rendering Provider
Standard Claim Processing Plan
- Process up to 500 claims and 300 ERAs per month with ease. Note: Workers' compensation claims are not included in this plan.
Low Volume
16.50Per Rendering Provider
Affordable Solution for Low-Volume Insurance Providers
- A cost-effective option designed for providers with only a few insured patients, offering up to 20 claims and 20 ERAs per month. Get the support you need without unnecessary expenses.
* The pricing here is for display purposes only. You should contact the partner for the most up to date and correct pricing information. We do not take any responsibility for this pricing information, which is provided by our partners. Pricing last updated: 07 Mar, 2025 12:00AM
Next Steps
Complete the enrollment form
Filling out the enrollment form helps us prepare your customer service agreement quickly and accurately.
Sign Customer Service Agreement
Review and sign the completed customer service agreement along with the agreed-upon fee schedule. Once signed, you'll be granted access to the portal.
Fill out the activate a partner form
Let both teams you're ready to activate the integration by using this form link.
Testimonials
Resources
FAQ
When a payer or clearinghouse rejection occurs, we update the claim status in Healthie, so you’re immediately aware of the issue. You can then search for the claim in our portal to see the exact error details. From there, you have the option to make edits directly in our portal using the claim editor or create a new claim in Healthie to resubmit with the necessary corrections.
Yes, we can save eligibility information back to Healthie! However, there are some caveats: each payer and plan may provide eligibility data in different formats. This means we'll work closely with you to identify the benefits you need saved, determine which payers return those benefits, and customize how we convert the data to fit your specific requirements.